For the roughly 1.5 million Americans per year who survive a traumatic brain injury, health outcomes vary widely. Not only can these injuries lead to a loss of coordination, depression, impulsivity, and difficulty concentrating, but they come with an amplified risk of developing dementia in the future.
The glaring absence of treatments for such a widespread condition drove a team of scientists at Gladstone Institutes to uncover, on a molecular level, how traumatic brain injuries trigger neurodegeneration—and, just as importantly, how to target that process to prevent long-term damage.
“We set out to address the fundamental question of exactly what happens in the brain after injury to ignite the damaging process that destroys neurons,” says Jae Kyu Ryu, Ph.D., a scientific program leader in the lab of Katerina Akassoglou, Ph.D. at Gladstone Institutes.
Most traumatic brain injuries come as a result of falls, car crashes, or violent assaults, according to the Centers for Disease Control, but many also stem from sports accidents or certain military operations such as explosions. In each case, the external force is strong enough to move the brain within the skull, causing a significant breakdown in the blood-brain barrier and allowing blood to move in.
“We knew that a specific blood protein, fibrin, was present in the brain after traumatic brain injury, but we didn’t know until now that it plays a causative role in brain damage after injury,” says Ryu, who led the study that appears in the Journal of Neuroinflammation.
Ryu and others in Akassoglou’s lab have long investigated how blood that leaks into the brain triggers neurologic diseases, essentially by hijacking the brain’s immune system and setting off a cascade of harmful, often irreversible effects. Fibrin, a protein that normally helps blood coagulate, is the culprit.
“Across many neurological diseases, toxic immune responses in the brain are triggered by blood leaks and drive neurodegeneration,” says Akassoglou, a senior investigator at Gladstone and the director of the Center for Neurovascular Brain Immunology at Gladstone and UCSF. “Neutralizing the toxic immune responses in the brain paves the way to new therapies for neurological diseases.”
In diseases such as Alzheimer’s and multiple sclerosis, abnormal leaks in the protective blood-brain barrier allow fibrin to seep into areas responsible for cognitive and motor functions, causing neurodegeneration. But in this case, the traumatic brain injury itself causes the blood to leak into the brain. The new study showed, for the first time, that fibrin is responsible for turning good immune cells bad, causing dangerous inflammation and unleashing toxins that kill neurons.
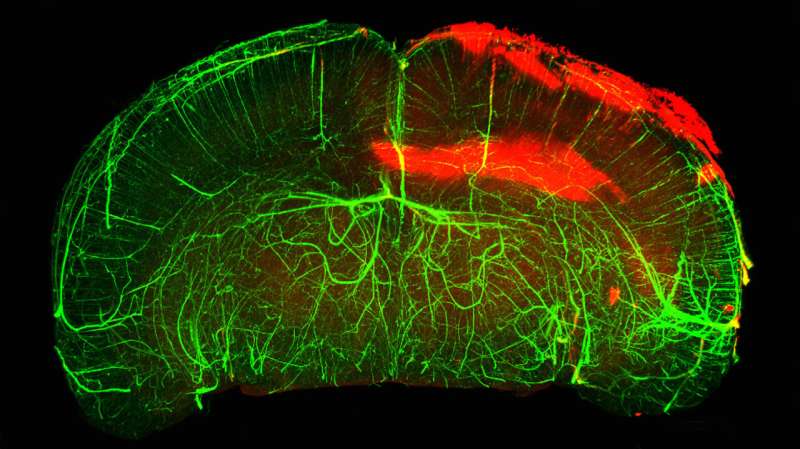
The Gladstone team used state-of-the-art imaging technology to study mouse brains, as well as brains from people who experienced a traumatic brain injury. They also produced three-dimensional imaging of a whole intact mouse brain, showing blood-brain barrier leaks and abundant fibrin in traumatic brain injury. In both mouse and human brains, fibrin was present together with activated immune cells.
“It became clear that fibrin is activating these immune cells,” Ryu says. “We realized that we could prevent the toxic effects if we could block fibrin, but we had to do it in a precise way.”
The team leveraged genetic tools with a specific mutation in fibrin that can block it from activating immune cells without affecting the protein’s beneficial blood-clotting abilities. This is especially critical for traumatic brain injuries, as excessive bleeding into the brain has been known to occur among patients who were taking anticoagulant medications before their injury.
Akassoglou’s lab previously developed a drug, a therapeutic monoclonal antibody, that acts only on fibrin’s inflammatory properties without adverse effects on blood coagulation. This fibrin-targeting immunotherapy protects from multiple sclerosis and Alzheimer’s disease in mice. A humanized version of this first-in-class fibrin immunotherapy is already in Phase 1 safety clinical trials by Therini Bio.
“It’s exciting to have a therapeutic option to neutralize blood toxicity in neurologic diseases,” Ryu says. “Future studies are needed to test the effects of the fibrin immunotherapy in traumatic brain injury.”
“This study identifies a potential new strategy to diminish the devastating impacts of brain injuries,” says Lennart Mucke, MD, director of the Gladstone Institute of Neurological Disease.
“Brain injuries can have profound effects on a person’s cognitive abilities, emotional health, and motor skills, touching every part of their life. It will be interesting to explore whether blocking the disease-promoting effects of fibrin can improve the outcome of brain surgeries and reduce disability when implemented after traumatic brain injuries have occurred.”
More information:
Terry Dean et al, Fibrin promotes oxidative stress and neuronal loss in traumatic brain injury via innate immune activation, Journal of Neuroinflammation (2024). DOI: 10.1186/s12974-024-03092-w
Citation:
A new therapeutic target for traumatic brain injury (2024, April 19)
therapeutic-traumatic-brain-injury.html
.
. The content is provided for information purposes only.
