Autoimmune conditions such as multiple sclerosis (MS) are disorders of the immune system associated in this case with demyelination of the central nervous system (CNS). The term demyelination describes damage to the layer covering nerve fibers in the brain and spinal cord.
Recently, medical researchers have been exploring the potential of treating these diseases by transplanting autologous hematopoietic cells or blood stem cells (i.e., immature cells found in the peripheral blood and bone marrow of patients). While this possible treatment has been the focus of various studies, its effects and cellular underpinnings remain poorly understood.
Researchers at Stanford University School of Medicine recently carried out a study aimed at better understanding how this treatment could act on the CNS in a mouse model of MS, called experimental autoimmune encephalomyelitis (EAE).
Their findings, published in Nature Neuroscience, suggest that the transplantation of hematopoietic cells could help to strengthen neuroprotective myeloid function, which could in turn lead to the improvement of neurological symptoms.
“The transplantation of patient-derived autologous hematopoietic cells is currently under investigation as a promising therapy option for treatment-resistant multiple sclerosis,” Marius Mader, lead author of the paper, told Medical Xpress. “However, so far not much is known about the underlying cellular or molecular processes within the central nervous system. This inspired us to explore the mechanisms that might lead to remission.”
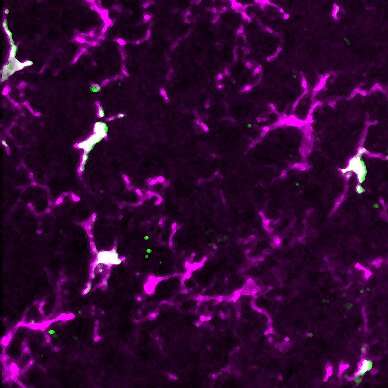
In their previous studies, Mader and his colleagues in the laboratory of senior author Marius Wernig, extensively studied the engraftment of peripheral hematopoietic cells into the brain. This is the process through which these cells differentiate towards the myeloid lineage, ending up resembling naïve microglia.
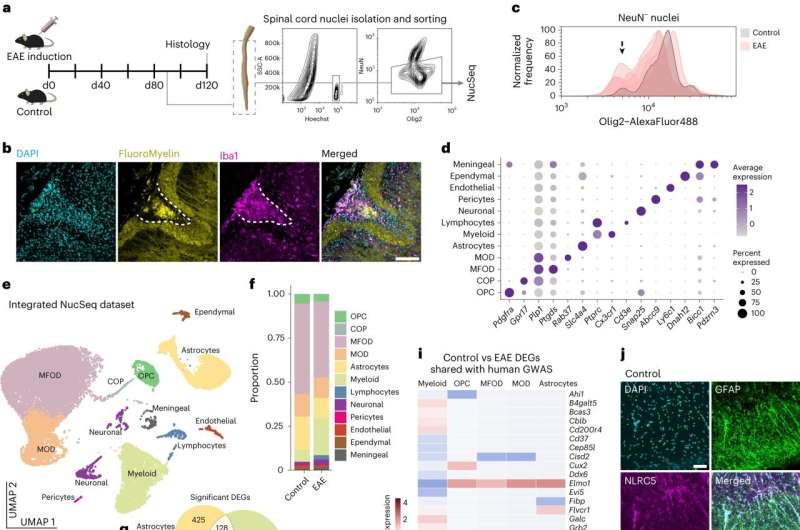
As part of their recent study, the researchers set out to investigate the possibility that a similar process also occurs after the transplantation of hematopoietic cells in EAE animals, hence specifically investigating the impact of transplantations on chronic neuroinflammatory diseases affecting the CNS.
“We modeled autologous hematopoietic cell transplantations, which are performed in human patients, by the transplantation of whole bone marrow cells in a mouse model of MS,” Mader explained. “In another experimental group, we combined this transplantation with the administration of a drug we previously found to increase the incorporation of donor-derived myeloid cells into the central nervous system, thus leading to a higher rate of microglia replacement.”
A further analysis method employed by Mader and his collaborators entailed isolating single nuclei from mouse spinal cord cells, to then extract and sequence their RNA. This technique allowed the researchers to examine the expression of genes in thousands of individual cells.
“We were thrilled to see that our model of hematopoietic cell transplantations led to a clinical improvement, hence providing preclinical support for this therapeutic strategy in line with the findings of clinical trials in multiple sclerosis patients,” Mader said. “This clinical effect was accompanied with reduced neuroinflammatory and increased neuroprotective molecular changes in different neural cell populations, such as astrocytes and oligodendrocytes.”
Remarkably, Mader and his colleagues found that by increasing the efficiency with which donor-derived myeloid cells underwent engraftment, using their microglia replacement approach, they could further consolidate the positive effects of cell transplantations. Following their interventions, they also observed significant changes in the composition of myeloid cell subpopulations.
Overall, the findings gathered by this research team suggest that hematopoietic cell transplantation could have positive effects on MS and other chronic inflammatory conditions affecting the CNS. In the future, they could thus pave the way for new clinical trials designed to further test this promising treatment option, potentially contributing to its widespread deployment.
“Our data suggests that the manipulation of the myeloid cell populations in the central nervous system might be a future therapeutic direction for chronic neuroinflammatory disorders,” Mader added. “We are motivated to further understand the biological basis and mechanisms that involve the recruitment and differentiation of peripheral hematopoietic cells in the brain and spinal cord.”
More information:
Marius Marc-Daniel Mader et al, Myeloid cell replacement is neuroprotective in chronic experimental autoimmune encephalomyelitis, Nature Neuroscience (2024). DOI: 10.1038/s41593-024-01609-3
© 2024 Science X Network
Citation:
How myeloid cell replacement could help treat autoimmune encephalomyelitis (2024, April 19)
myeloid-cell-autoimmune-encephalomyelitis.html
.
. The content is provided for information purposes only.
