In the past decade, immunotherapy has emerged as the fourth pillar of cancer treatment, joining surgery, radiotherapy and chemotherapy. It is an approved treatment for 15 cancers, including melanoma and some types of lymphomas and leukemias, but it is not effective in all cancers or in all patients.
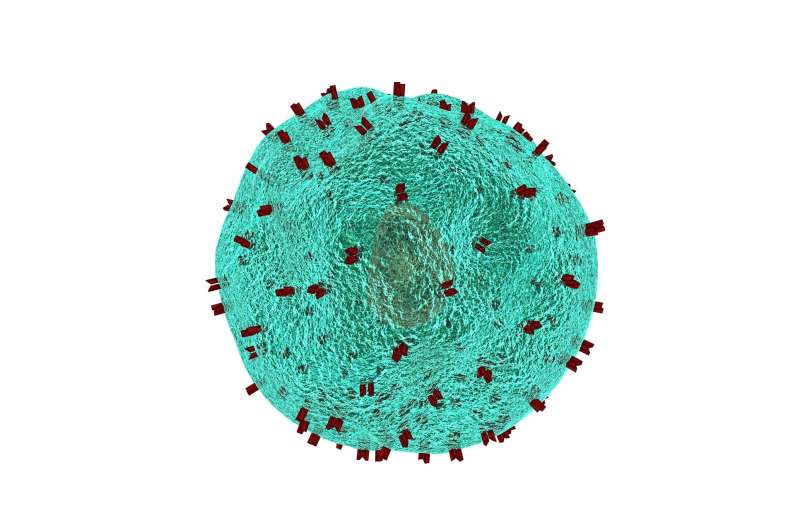
Immunotherapy uses a patient’s own cancer-fighting cells, or T-cells, and adapts them so that they do a better job at killing cancer cells. T-cells are excellent at identifying and attacking tumor cells but can become exhausted in the tumor microenvironment, where they can become overworked and overstimulated, and are starved of glucose and other nutrients by tumor cells. Helping these cells to function better and live longer could improve immunotherapy responses.
“T-cell exhaustion has been a key factor in preventing optimal responses to immunotherapy,” said Shikhar Mehrotra, Ph.D. co-leader of the Cancer Biology & Immunology Research Program and scientific director of the Center for Cellular Therapy at MUSC Hollings Cancer Center.
Research in the Mehrotra Lab suggests that overcoming T-cell exhaustion could improve responses to two types of immunotherapies—anti-PD1 therapy and CAR-T therapy.
In a recent study reported in the Proceedings of the National Academy of Sciences, Mehrotra and his team, which included Shilpak Chatterjee, Ph.D., showed that T-cell exhaustion limited the efficacy of anti-PD1 therapy. That therapy works by unmasking tumor cells, allowing T-cells to see and target them.
The study showed that T-cells expressing the cell receptor CD38 were more susceptible to exhaustion. Using an anti-CD38 antibody, the research team was able to block CD38 and overcome T-cell exhaustion. They then showed in a mouse model that overcoming T-cell exhaustion by blocking CD38 restored the efficacy of anti-PD1 therapy against cancer. However, the anti-CD38 antibody they used in the mouse model would not be appropriate for use in humans.
To find a way to combat T-cell exhaustion in humans, and specifically for CAR-T therapy, Mehrotra and Chatterjee have developed and patented a cytokine “cocktail” that can be used to reduce CD38 expression on T-cells. In CAR-T therapy, the patient’s own immune cells are harvested, enhanced to detect and fight the cancer cells more effectively and then put back into the patient.
Although the processing of these cells outside the body makes them better able to fight cancer, it also exhausts them, making it difficult for them to survive long in the nutrient-depleted tumor microenvironment. Treating the cells with the cytokine cocktail while they are out of the body not only reduces their expression of CD38, a marker of exhaustion, but it also helps to ensure their function and longevity by giving them the traits of both Th1 (effector) and Th17 (stemness) cells.
Th1 cells can mount an anti-cancer response but are short-lived, while Th17 cells have greater longevity but are unable to mount a response. Combining the two harnesses the strengths of both, producing T-cells that live longer and can mount an effective response. These cells are also less likely to depend on glucose and better able to withstand the nutrient-deprived tumor microenvironment.
Mehrotra believes that the cocktail could be an important key to overcoming exhaustion in T-cells, ensuring their long-term effectiveness and improving responses to immunotherapy.
“In the clinical setting, we want these T-cells to be ‘marathon runners,’ not sprinters in a 100-meter dash,” said Mehrotra.
The cocktail is currently being used in a phase 1 clinical trial of CD19 CAR-T-cells in adult patients with certain relapsed or refractory B-cell cancers. It allows the cells to continue dividing and remain persistent as they attack the tumor environment.
Thus far, two patients have been enrolled and both have tolerated the treatment well and achieved complete responses without experiencing any of the side effects that are otherwise commonly associated with CAR-T-cell therapy. Based on these results, a second set of patients is being enrolled in this trial, which is now open at MUSC’s Hollings Cancer Center.
More information:
Anwesha Kar et al, CD38–RyR2 axis–mediated signaling impedes CD8 + T cell response to anti-PD1 therapy in cancer, Proceedings of the National Academy of Sciences (2024). DOI: 10.1073/pnas.2315989121
Citation:
Improving cancer immunotherapy by prolonging T-cell survival (2024, April 22)
retrieved 23 April 2024
cancer-immunotherapy-prolonging-cell-survival.html
.
. The content is provided for information purposes only.
