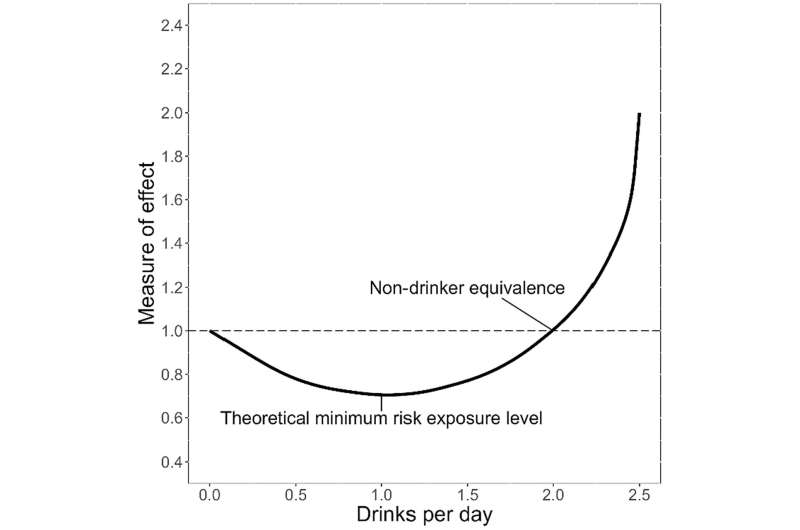
Low to moderate drinking may not be protective against certain health conditions, and “safe” alcohol use guidelines may be substantially off base. These are among the implications of a review of studies that use a novel research method. For most health conditions, the evidence that any amount of drinking increases risk is strong. For some other diseases, however, traditional data analysis yields a J-curve effect.
In these findings, low-to-moderate drinking coincides with the lowest disease risk, while abstainers have a slightly higher risk, and heavy drinkers have a much greater risk. That’s why a limited amount of red wine, which is high in antioxidants, has been considered protective against certain types of heart disease, type 2 diabetes, dementia, and depression.
The premise that alcohol in smaller amounts has health benefits, somewhat offsetting its harms at higher doses, is built into models of alcohol’s individual and societal effects and costs and public health policy and drinking guidelines. The J-curve effect is facing increasing scrutiny of biases that may be contributing to it. The key challenge for researchers is establishing causation.
Alcohol studies are observational; ethical and practical barriers prevent randomized controlled trials. However, observational studies are subject to biases, especially to do with “confounders”—like socioeconomic status and other hard-to-measure factors that may influence health outcomes.
Recent advances in statistical approaches, combined with increasing availability of large data sets, offer ways to use observational data that more closely resemble randomized controlled trials. For the new review published in Alcohol: Clinical & Experimental Research, investigators in Australia compared findings using more novel methodologies to findings from traditional approaches exploring alcohol’s effect on long-term disease outcomes.
One of the methods the researchers focused on was Mendelian Randomization (MR). This approach relates genetically predicted exposure levels (e.g., alcohol use) to health outcomes (e.g., a specific disease). Genetic analysis is especially appropriate for scrutinizing J-shaped curves of alcohol’s health effects.
For example, the MR approach suggests that alcohol at low levels may still be protective for certain conditions, such as type 2 diabetes—but its protective effects now seem much smaller and the risk much bigger than traditional methods suggested. For cardiovascular disease, the perceived benefits of alcohol disappear.
An MR evaluation of alcohol and all-cause mortality in men also found no protective effects of alcohol, a finding that contrasts with observational analysis of the same population sample. Improving our understanding of alcohol’s long-term effects is crucial for policy and practice.
Even if the protective effect of drinking is confirmed to be causal for some health outcomes, it is likely small and more than offset by alcohol’s harms. Discrediting the J-curve could have substantive effects on drinking guidelines. In Australia, the number of drinks per week associated with acceptable health risks could fall from 10 to 2.5.
Clinical guidance on alcohol risk may need to be tailored to individuals, depending on their underlying risk factors and demographic characteristics. The researchers call for greater focus on the mechanisms by which alcohol may exert some protection, since this could help identify alternatives. For example, if alcohol in low amounts modifies cardiovascular risk by reducing platelet activity, aspirin can achieve that without the risks of drinking.
Potentially, any protective effects of alcohol could be reframed as proof of concept for lifestyle interventions. The researchers acknowledge that even novel approaches to exploring causality are imperfect. Triangulating multiple analytical methods with complementary strengths and weaknesses is the most promising route to understanding alcohol’s long-term health effects
More information:
Rachel Visontay et al, Is low?level alcohol consumption really health?protective? A critical review of approaches to promote causal inference and recent applications, Alcohol: Clinical and Experimental Research (2024). DOI: 10.1111/acer.15299
Citation:
Low levels of alcohol may not be healthy after all, according to new analytical approaches (2024, April 22)
alcohol-healthy-analytical-approaches.html
.
. The content is provided for information purposes only.
