Smokers who have small abnormalities on their CT scans that grow over time have a greater likelihood of experiencing acute respiratory disease events, according to a new study published in Radiology.
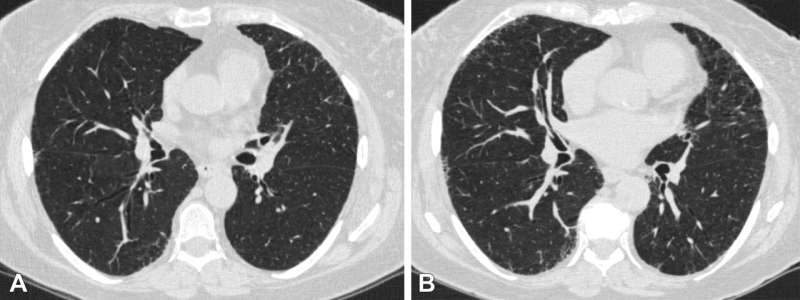
Quantitative interstitial abnormalities (QIA) are subtle abnormalities on chest CTs that do not meet the diagnostic criteria for advanced pulmonary diseases but are nonetheless associated with decreased lung function and capacity, increased respiratory symptoms and death.
“QIA includes features like reticulation and ground-glass opacities as well as subtle density changes with important clinical implications,” said Bina Choi, M.D., associate physician in the Division of Pulmonary and Critical Care Medicine at Brigham and Women’s Hospital and postdoctoral fellow at the Applied Chest Imaging Laboratory, Harvard Medical School in Boston.
“In some patients, QIA may be a precursor to advanced diseases such as pulmonary fibrosis or emphysema.”
Acute respiratory disease events are episodes of increased cough, phlegm or shortness of breath that last at least two days and require treatment with steroids or antibiotics. Severe acute respiratory disease episodes require an emergency room visit or hospitalization.
“We wanted to determine whether progression in QIA on chest CT is associated with acute respiratory disease events in individuals with a history of smoking,” Dr. Choi said. “While many acute respiratory disease events are likely related to airway disease and COPD, some may instead be associated with QIA, especially in people without obstruction or emphysema.”
Dr. Choi’s team performed a secondary analysis of the CT scans of 3,972 participants (mean age 60.7; 2,120 women) in the COPDGene Study, one of the largest studies ever to investigate the underlying genetic factors of COPD. The study included individuals with a 10-pack-year or greater smoking history recruited from multiple centers between November 2007 and July 2017.
QIA was measured with machine learning-based tools as a percentage of lung volume on a CT scan. QIA progression was assessed using the participants’ QIA measurements at baseline and five-year follow-up CT exams.
Statistical analyses revealed that participants in the highest quartile of QIA progression had more frequent acute respiratory disease and severe acute respiratory disease events than those in the lowest quartile.
“We found that progression in QIA is independently associated with these acute respiratory disease events both intercurrent and subsequent to progression,” she said.
Dr. Choi said the results suggest that QIA progression may represent changes in lung tissue processes that have both short- and long-term impacts on patient symptoms and the worsening of those symptoms.
“Severe acute respiratory disease events may be a sign of disease activity and a source of morbidity at the earliest stages of lung tissue injury,” she said. “Some people with QIA progression may merit more aggressive monitoring and earlier intervention.”
More information:
Association of Acute Respiratory Disease Events with Quantitative Interstitial Abnormality Progression at CT in Individuals with a History of Smoking, Radiology (2024).
Citation:
Lung abnormality progression linked to acute respiratory disease in smokers (2024, April 30)
lung-abnormality-linked-acute-respiratory.html
.
. The content is provided for information purposes only.
